Leslie RBHR Dr. Poole September 2009
|
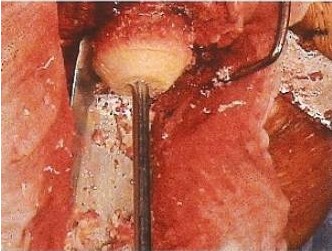
I am a 57-year-old female who had her right hip resurfaced by Dr. Colin Poole of Boise, Idaho, about 5 weeks ago. I want to share my story, as so many have, as a way of “paying it forward” in appreciation of the guidance and inspiration I received from so many who have already posted here. The first indication that I had anything wrong appeared quite abruptly 3 ½ years ago, when I was diagnosed with sacroiliac joint dysfunction. I suddenly could not walk upstairs – or anywhere else, for that matter – without excruciating pain in my right lower back. Before long, pain radiated to my right hip, knee, thigh, and buttocks, until at some point everything from my bellybutton to my ankle was screaming at me. A physical therapist eventually connected the dots on the initial diagnosis, explaining that my back was compensating for what my hip couldn’t do, resulting in the overload that masqueraded as a back problem. I consulted with Dr. Poole, who took an X-ray that indicated no significant arthritis. He wisely suggested at that point that I get an MRI, and I unwisely chose not to. Thus began my painful 3-year quest to avoid surgery at all costs. I sought treatment from an army of physical therapists, a massage therapist, a rolfer, a gal calling herself an orthobionomist (don’t ask), a sports doctor, and a chiropractor. All meant well and did their best (with the exception of the chiropractor, for whom the term “quack” is an insult to ducks. The lesson to pass on from him is that if anyone promises you they can grow your cartilage back in 2-3 years, as he did, grab your wallet and run for the nearest exit). After no lasting relief, the sports doctor finally convinced me to get the MRI, which showed significant degeneration in the hip. Knowing I had exhausted every other alternative at my disposal, I threw in the towel and scheduled the surgery. It’s worth noting that three years ago, my husband had a hip resurfacing done by Dr. Poole – in fact, same hip, same hospital, and even at the same age as me (be careful who you marry; you never know what you’ll wind up sharing!) – so I had been through the entire process as an observer and caregiver. Suffice it to say that my husband has been a very happy camper ever since his surgery, which made it that much easier for me to accept the inevitable. The Procedure By the morning of the surgery, I was so certain this was what I had to do that I was not only ready, but almost eager. The surgery went smoothly, and resulted in a couple of interesting surprises: First, Dr. Poole discovered an unexpected cyst, which he was able to remove without incident. Second, and more important, he found a pebble-sized chunk of bone that had been floating around in my hip, that hadn’t appeared either on the X-ray or MRI (see picture below). Apparently there had been a significant trauma that chipped off a piece of bone, acting as a major contributor to my cartilage loss. The other contributing factor is that I have a mild case of hip dysplasia. I may never know which ultimately caused my hip to go south. Bone chip being removed from hip joint
Pleasant Surprises
We all go into surgery as a last resort, aware of the risks we are assuming,
and often fearfully anticipating what the recovery will be like. Happily,
this is a summary of all the things that went much better than my worst
imaginings.
1) Many of the restrictions I assumed I had to follow during recovery turned
out to apply only to total hip replacement patients, not resurfacing. The
literature my hospital gives hip patients to review pre-op still doesn’t
fully address the differences between THR and BHR. I was thrilled to learn,
for instance, that I could both squat and bend from the waist during
recovery, as avoiding those seemed like pretty daunting challenges.
2) Sleeping on my back post-op, which I could almost never do beforehand,
suddenly was not a problem at all. What a relief!
3) I never expected to nap as much as I did the first couple of weeks, and I
haven’t been a napper since infancy – but boy, that was a deep and
refreshing sleep when I was zonking out for a couple of hours in the middle
of the afternoon every day.
4) The automatic foot-squeezer machine in the hospital turned out to feel
mostly like a pleasant massage. (Okay, it did wake me up a few times – but
mostly it felt pretty good.)
5) One of the biggest, most pleasant surprises was courtesy of my physical
therapist at the hospital. The first time he got me up and ambulatory after
surgery, watching me wobble down the hospital corridor with my walker, he
commented, “You’re doing fine with the walker. But the truth is, you could
walk unassisted starting right now if you wanted to.” When he saw the shock
on my face, he added, “Really! I see resurfacing patients leave the hospital
unassisted all the time.” Wow! Here I was, assuming I’d need a walker for
the standard couple of weeks, then crutches, then a cane until about 6 weeks
post-op. I pretty much did what he suggested, and have been walking
unassisted almost since I got home. I still take a cane on longer walks
(I’ve been going 1-2 miles a day since 2-3 weeks post-op), or when I feel
fatigued, or in crowded public places where I just want to alert others to
give me margin. My PT says that should last another week or so.
6) I wasn’t sure how quickly I could negotiate stairs, but that has turned
out to be in almost no time. We have a two-story house, so it’s been great
being able to get up and down so quickly.
Unpleasant Surprises
I would never want to mislead anyone into thinking this was all fun and
games, so here are the things that turned out to be not so pleasant:
1) I never expected the amount of bruising that covered my leg for the first
3 weeks or so. It wasn’t even black and blue; it was charcoal black, and
covered such an alarming area that I called Dr. Poole’s office to make sure
it was normal. (It was.) Some people have swelling – I only had a little; my
husband had a ton – and some bruise. No way to predict it. The bruising
didn’t hurt, but it sure looked awful.
2) The nausea from all the meds surprised me. The first time I was upright
after surgery, I was pretty green around the gills. The ginger ale a nurse
brought was a great help.
3) I was initially pleased when Dr. Poole told me I didn’t need to donate
any of my own blood prior to the surgery, as he found that patients under
age 64 lose so little blood that he never needs it. Well, almost never.
Turns out I lost enough blood that after surgery my hematocrit level was
quite low. Dr. Poole first recommended a transfusion – meaning someone
else’s blood – but when I expressed my concern over the risks, he agreed
that we could go with a potent iron supplement. Which leads us to our last
unpleasant surprise, which is…
4) Potent iron supplements have nasty side effects. I was thrilled when Dr.
Poole took me off them.
Things I’m Glad I Didn’t Buy Before Surgery
1) A fancy shower chair. Our plastic, stackable lawn chair worked just fine.
2) The Polar Care 300, or Ice Man. I know that people love this, but my
hospital only had them for knee patients, and the local medical supply house
sold them for well over $200. The 10 X 15 ice pack I had purchased for $13 –
which I highly recommend, since you can wrap it around your hip and it stays
cold for hours – was a very decent substitute..
3) Silk sheets or silk pajamas, for ease of movement in and out of bed. I
found our smooth, nicely worn percale sheets worked great.
4) The sock putter-on-er, or reacher. Once I realized I could bend over
during recovery, the reacher became irrelevant, and I found I could put
socks on fine by bending my foot up behind me and fumbling around with it
from that angle.
Other Tips and Lesson Worth Sharing
1) Don’t put too much stock in DEXA scans – and if yours are not so great,
as was the case with me, see if you can get a surgeon who’s not rigid about
them. I had reason to be skeptical of my scan results, as I had gone to two
different machines within a month or so of each other, and got wildly
different results. Why aren’t they calibrated the same -and which do you
believe? Add that to not knowing what group of people you’re being compared
to, the potential for technicians’ errors, the fact that they don’t correct
at all for patient size (meaning large people get results that are too high,
and petite people – like me – get results that are too low), and you begin
to see why these are controversial, and not an exact science. Bottom line
with me is that I went in with a DEXA reading of severe osteopenia, but came
out with Dr. Poole’s proclamation that my bones were just fine. He even took
a picture during surgery so I could see for myself:
Bone chip being removed from hip joint
Pleasant Surprises
We all go into surgery as a last resort, aware of the risks we are assuming,
and often fearfully anticipating what the recovery will be like. Happily,
this is a summary of all the things that went much better than my worst
imaginings.
1) Many of the restrictions I assumed I had to follow during recovery turned
out to apply only to total hip replacement patients, not resurfacing. The
literature my hospital gives hip patients to review pre-op still doesn’t
fully address the differences between THR and BHR. I was thrilled to learn,
for instance, that I could both squat and bend from the waist during
recovery, as avoiding those seemed like pretty daunting challenges.
2) Sleeping on my back post-op, which I could almost never do beforehand,
suddenly was not a problem at all. What a relief!
3) I never expected to nap as much as I did the first couple of weeks, and I
haven’t been a napper since infancy – but boy, that was a deep and
refreshing sleep when I was zonking out for a couple of hours in the middle
of the afternoon every day.
4) The automatic foot-squeezer machine in the hospital turned out to feel
mostly like a pleasant massage. (Okay, it did wake me up a few times – but
mostly it felt pretty good.)
5) One of the biggest, most pleasant surprises was courtesy of my physical
therapist at the hospital. The first time he got me up and ambulatory after
surgery, watching me wobble down the hospital corridor with my walker, he
commented, “You’re doing fine with the walker. But the truth is, you could
walk unassisted starting right now if you wanted to.” When he saw the shock
on my face, he added, “Really! I see resurfacing patients leave the hospital
unassisted all the time.” Wow! Here I was, assuming I’d need a walker for
the standard couple of weeks, then crutches, then a cane until about 6 weeks
post-op. I pretty much did what he suggested, and have been walking
unassisted almost since I got home. I still take a cane on longer walks
(I’ve been going 1-2 miles a day since 2-3 weeks post-op), or when I feel
fatigued, or in crowded public places where I just want to alert others to
give me margin. My PT says that should last another week or so.
6) I wasn’t sure how quickly I could negotiate stairs, but that has turned
out to be in almost no time. We have a two-story house, so it’s been great
being able to get up and down so quickly.
Unpleasant Surprises
I would never want to mislead anyone into thinking this was all fun and
games, so here are the things that turned out to be not so pleasant:
1) I never expected the amount of bruising that covered my leg for the first
3 weeks or so. It wasn’t even black and blue; it was charcoal black, and
covered such an alarming area that I called Dr. Poole’s office to make sure
it was normal. (It was.) Some people have swelling – I only had a little; my
husband had a ton – and some bruise. No way to predict it. The bruising
didn’t hurt, but it sure looked awful.
2) The nausea from all the meds surprised me. The first time I was upright
after surgery, I was pretty green around the gills. The ginger ale a nurse
brought was a great help.
3) I was initially pleased when Dr. Poole told me I didn’t need to donate
any of my own blood prior to the surgery, as he found that patients under
age 64 lose so little blood that he never needs it. Well, almost never.
Turns out I lost enough blood that after surgery my hematocrit level was
quite low. Dr. Poole first recommended a transfusion – meaning someone
else’s blood – but when I expressed my concern over the risks, he agreed
that we could go with a potent iron supplement. Which leads us to our last
unpleasant surprise, which is…
4) Potent iron supplements have nasty side effects. I was thrilled when Dr.
Poole took me off them.
Things I’m Glad I Didn’t Buy Before Surgery
1) A fancy shower chair. Our plastic, stackable lawn chair worked just fine.
2) The Polar Care 300, or Ice Man. I know that people love this, but my
hospital only had them for knee patients, and the local medical supply house
sold them for well over $200. The 10 X 15 ice pack I had purchased for $13 –
which I highly recommend, since you can wrap it around your hip and it stays
cold for hours – was a very decent substitute..
3) Silk sheets or silk pajamas, for ease of movement in and out of bed. I
found our smooth, nicely worn percale sheets worked great.
4) The sock putter-on-er, or reacher. Once I realized I could bend over
during recovery, the reacher became irrelevant, and I found I could put
socks on fine by bending my foot up behind me and fumbling around with it
from that angle.
Other Tips and Lesson Worth Sharing
1) Don’t put too much stock in DEXA scans – and if yours are not so great,
as was the case with me, see if you can get a surgeon who’s not rigid about
them. I had reason to be skeptical of my scan results, as I had gone to two
different machines within a month or so of each other, and got wildly
different results. Why aren’t they calibrated the same -and which do you
believe? Add that to not knowing what group of people you’re being compared
to, the potential for technicians’ errors, the fact that they don’t correct
at all for patient size (meaning large people get results that are too high,
and petite people – like me – get results that are too low), and you begin
to see why these are controversial, and not an exact science. Bottom line
with me is that I went in with a DEXA reading of severe osteopenia, but came
out with Dr. Poole’s proclamation that my bones were just fine. He even took
a picture during surgery so I could see for myself:
|